Diabetic Retinopathy: Symptoms and Diagnosis
Diabetes is a health condition where the body produces lower insulin levels than needed to manage blood sugar. High blood sugar can cause many problems in our bodies. Even though diabetes does not have a full-fledged cure, it can be controlled by maintaining a healthy lifestyle. It is also necessary to look out for symptoms of problems caused by diabetes, such as diabetic retinopathy.
What is Diabetic Retinopathy?
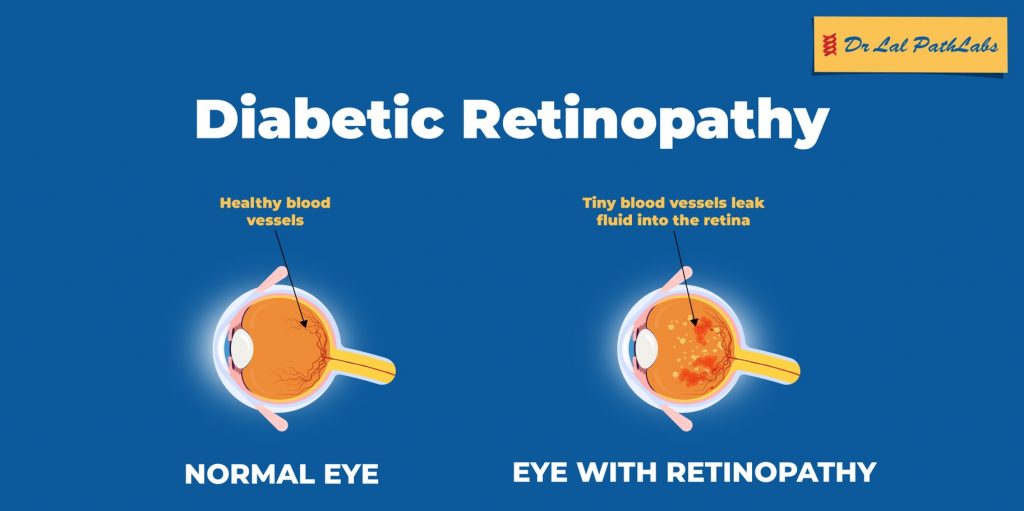
Diabetic retinopathy is a diabetic eye problem caused by high blood sugar levels that can cause damage to the blood vessels near the retina, the part of the eye where an image is formed. Diabetic retinopathy can cause loss of vision or even blindness. Therefore, people with diabetes must manage blood sugar levels and get a regular eye check-up done to manage this condition.
Stages of Diabetic Retinopathy
The two types of diabetic retinopathy that affect patients with diabetes are nonproliferative and proliferative. Nonproliferative (NPDR) refers to the early stages of diabetic retinopathy, whereas proliferated indicates severe damage. Proliferative is the final stage of diabetic retinopathy. Here is a breakdown of all four stages:
Stage 1: Mild Nonproliferative Diabetic Retinopathy
Mild nonproliferative is the first stage of diabetic retinopathy. In this stage, the patient does not experience any symptoms. An eye examination can detect it. In the first stage, tiny bulges appear on the retina, known as microaneurysms. These bulges might cause a small amount of blood leakage into the retina. The doctor will recommend an eye check-up every twelve months at this stage.
Stage 2: Moderate Nonproliferative Diabetic Retinopathy
Moderate Nonproliferative Diabetic Retinopathy, also called pre-proliferative retinopathy, is the second stage. This stage is characterised by swelling in the blood vessels near the retina. As a result, the blood vessels are unable to carry blood as they did before which leads to physical changes in the retina.
The changes caused during the second stage might cause diabetic macular edema (DME) in some people, which is a condition that causes blood and other fluids to accumulate in the macula. Macula is responsible for straight-ahead vision. The second stage is a warning sign that diabetic eye disease can cause damage to the vision. The doctor will conduct eye check-ups every 3-6 months at this stage.
Stage 3: Severe Nonproliferative Diabetic Retinopathy
In the third stage, there is a severe blockage to the blood flow from reaching the retina. The lack of blood flow causes the body to send signals to the brain to grow more blood vessels in this area. However, these new blood vessels formed are fragile and can cause bleeding.
Moreover, if the blood vessels close altogether, it can lead to macular ischemia. At this stage, the patients might suffer from blurry vision with dark spots. Vision loss at severe nonproliferative diabetic retinopathy is irreversible. However, treatment to stop further vision loss is available.
Stage 4: Proliferative Diabetic Retinopathy
Proliferative diabetic retinopathy is an advanced stage where the growth of the fragile blood vessels near the retina continues. Eventually, the bleeding also resumes, causing scar tissue to form. The scar tissue causes retinal detachment, leading to permanent loss of straight-ahead and side vision.
Symptoms of Diabetic Retinopathy
During the early stages, there are no visible symptoms of diabetic retinopathy. The symptoms start to appear in the final stage. Diabetic retinopathy is a severe diabetic eye disease, so you must look out for the following symptoms:
- Blurry vision
- Fluctuating vision
- Empty areas in the vision
- Floating dark spots or strings in the vision
- Loss of vision
- Decrease in the field of vision
Diabetic Retinopathy Diagnosis
Since the symptoms of diabetic retinopathy do not appear in the early stages, it is recommended that diabetic patients get their eyes screened at least once a year. Here is how the doctor may diagnose diabetic retinopathy:
- Eye screening
- Testing the pressure in the eyes
- Optical Coherence Tomography (OCT) uses light to take pictures of the inside of the eye.
- A Fluorescein angiogram involves injecting a dye into your veins and then taking photos of the eye to detect any damage to the blood vessels.
Depending on the diagnosed stage, the doctor might use one or more methods to ensure a proper diagnosis.
Treatment of Diabetic Retinopathy
While the loss of vision due to diabetic retinopathy is permanent, it is possible to avoid future damage by making the right choices. If this condition is detected early without any damage to the retina, it is possible to treat it by maintaining a healthy blood sugar level.
Here are some treatments available for diabetic retinopathy:
- Steroid eye injections can stop inflammation and reduce the growth of new blood vessels.
- Photocoagulation or laser surgery to reduce swelling and prevent fragile blood vessels from developing.
- Vitrectomy is a surgical treatment to remove the vitreous gel.
- Laser coagulation to seal the bleeding of the blood vessels.
Our eyes are a significant part of how we perceive the world, and we must take good care of them. Daily exercise and a balanced diet can regulate blood sugar levels, which are crucial for preventing diabetic retinopathy. Also, make sure to take the prescribed diabetes medicines on time and get your eyes checked by a doctor at least once every year.
Remember, prevention is better than cure. Understanding how to manage diabetes well is the key to preventing severe damage to your body.