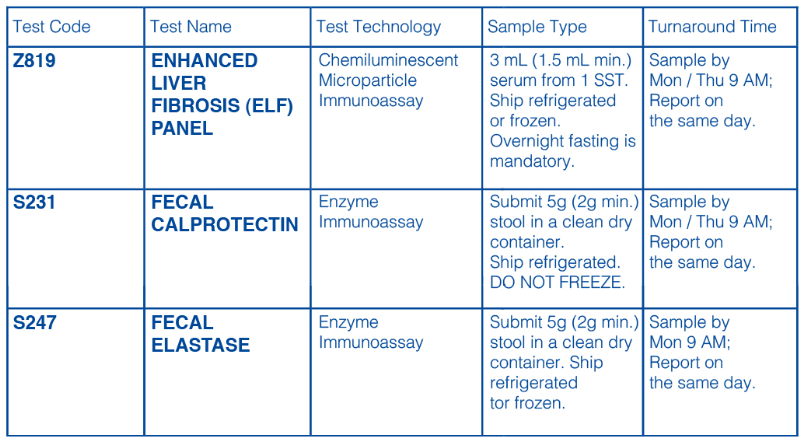
Three Major Diagnostic Tests for Gastrointestinal Problems

GIVE YOUR PATIENT AN ACTIVE AND A HEALTHY LIFESTYLE WITHOUT GASTROINTESTINAL WOES
ENHANCED LIVER FIBROSIS: ITS ASSOCIATION WITH NON-ALCOHOLIC FATTY LIVER DISEASE (NAFLD) AND LIVER FIBROSIS
Liver fibrosis is a consequence of various Chronic Liver Diseases, often caused by viruses, alcohol, fat deposition and can result in liver cirrhosis.
Cirrhosis is the main cause of morbidity and mortality in Chronic Liver Disease, but is often asymptomatic until the functions of the liver are completely compromised or portal hypertension develops. Also, for chronic viral hepatitis, the degree of liver fibrosis is an important parameter for decisions on antiviral therapy. Hence, the early detection of fibrosis progression and the development of cirrhosis are important in the management of patients with Chronic Liver Disease.
A Liver biopsy remains the reference standard for evaluating liver fibrosis. However, it has certain limitations:
• Sampling error
• Risk of complications
• Misinterpretation of the fibrosis stage
• Biopsy specimen represents only 1/50,000th of the total liver mass
• Cirrhosis can be understaged in 10-30% of cases
• Resampling is difficult because of the invasive nature and complications, such as pain and bleeding especially when repeated examinations are required to monitor the response to antiviral or anti-fibrosis treatment
The Enhanced Liver Fibrosis Test Panel is a promising non-invasive alternative to determine liver fibrosis and cirrhosis. The test has better automaticity, has high reproducibility, less invasiveness and proven considerable diagnostic performance. The test has received the Conformite Europeenne (CE) mark and the staging of liver fibrosis has been validated in patients with Chronic Hepatitis C, Alcoholic Liver Disease and Non-alcoholic Fatty Liver Disease.
The test uses an algorithm of three serum biomarkers found in the blood to calculate an ELF score:
• Hyaluronic Acid
• Procollagen III Amino Terminal Peptide
• Tissue Inhibitor of Metalloproteinase 1
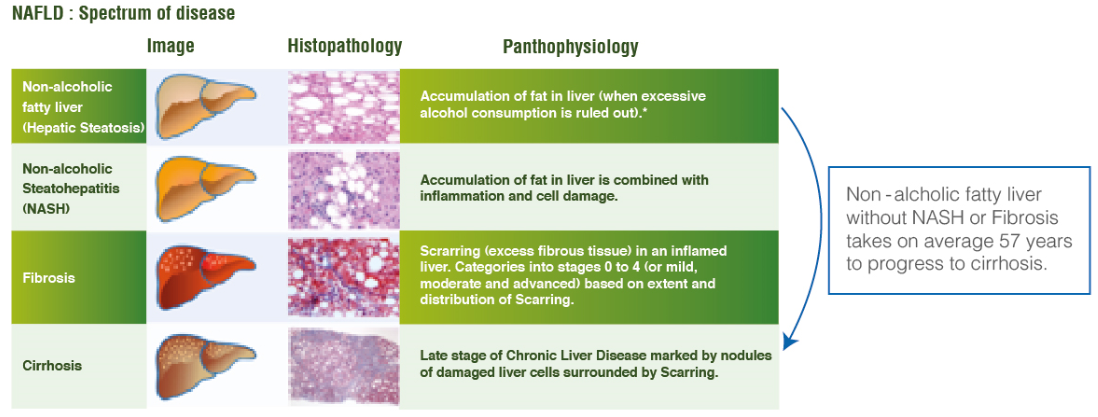
Non-alcoholic Fatty Liver Disease (NAFLD) is a spectrum of disease from fatty liver to non-alcoholic steatohepatitis, fibrosis, and cirrhosis depicted below in Figure 1 (Glen et al. 2016).
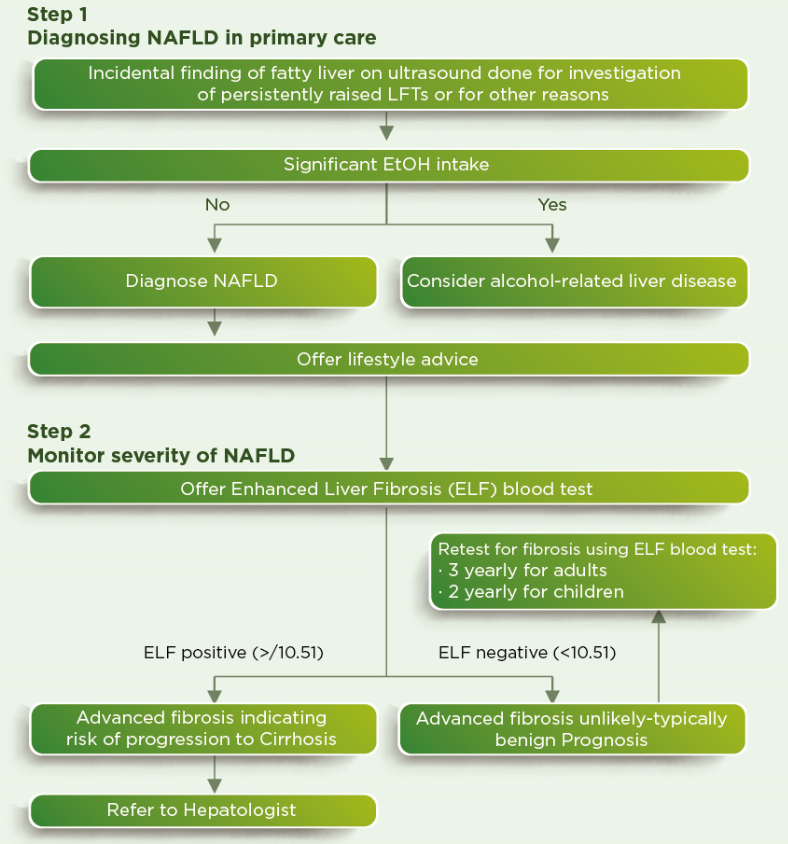
The Testing protocol for NAFLD w.r.t the NICE guidelines and Guideline Development Group (GDG) is as follows:
References:
1.Xie, Q. et al. The performance of enhanced liver fibrosis (ELF) test for the staging of liver fibrosis: a meta-analysis. PLoS ONE 9, e92772 (2014).
2.Catanzaro, R. et al. Diagnostic accuracy of enhanced liver fibrosis test to assess liver fibrosis in patients with chronic hepatitis C. HBPD INT 12, 500-507 (2013).
3.Friedrich-Rust, M. et al. Comparison of ELF, FibroTest and FibroScan for the non-invasive assessment of liver fibrosis. BMC Gastroentero110, 103 (2010).
4.Kim, B. K. et al. Prospective validation of ELF test in comparison with Fibroscan and FibroTest to predict liver fibrosis in Asian subjects with chronic hepatitis B. PLoS ONE 7, e41964 (2012).
5.Rosenberg, W. M. C. et al. Serum markers detect the presence of liver fibrosis: a cohort study. Gastroenterology 127, 1704-1713 (2004).
6.Guha, I. N. et al. Noninvasive markers of fibrosis in Non-alcoholic fatty liver disease: Validating the European Liver Fibrosis Panel and exploring simple markers. Hepatology 47, 455-460 (2008).
7. Glen, J., Floros, L., Day, C. & Pryke, R. Non-alcoholic fatty liver disease (NAFLD): summary of NICE guidance. BMJ 354, i4428 (2016).
FECAL CALPROTECTIN
In clinical practice, distinguishing between Irritable Bowel Syndrome (IBS) and organic gastrointestinal diseases, notably chronic Inflammatory Bowel Disease (IBD), is challenging as there is an overlap in the symptoms. Sensitive, accurate and non-invasive markers that can help in the diagnosis are thus of great importance. Furthermore, monitoring of the patients to adapt treatment in case of relapse or aggravation is also of crucial importance.
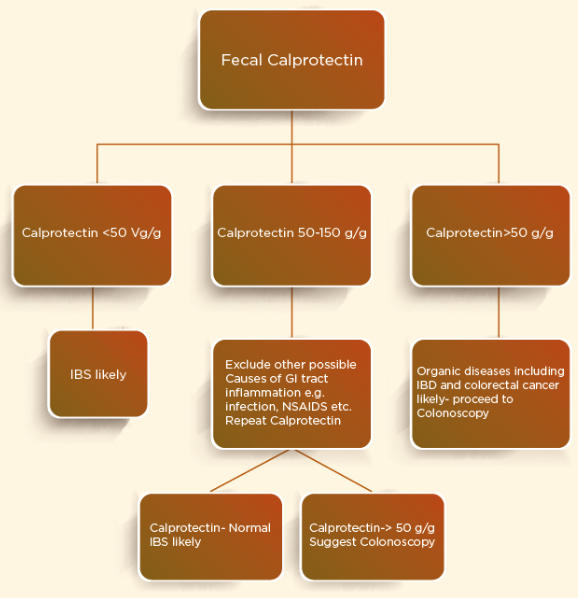
Fecal Calprotectin (CPN) is one such reliable and inexpensive test of high sensitivity and specificity that helps the diagnosis of Inflammatory Bowel Disease and also helps to determine the disease activity and treatment response as depicted in Figure 2 (Manceau et al. 2016).

As per the NICE guidelines the protocol to be followed for testing and use of Fecal Calprotectin is as follows:
References:
1. Erbayrak, M. et al. The Role of Fecal Calprotectin in Investigating Inflammatory Bowel Diseases. Clinics (Sao Paulo) 64,421-425 (2009).
2. Manceau, H., Chicha-Cattoir, V., Puy, H. & Peoc’h, K. Fecal calprotectin in inflammatory bowel diseases: update and perspectives. Clinical Chemistry and Laboratory Medicine (CCLM) 55,474-483 (2016).
3. Alibrahim, B., Aljasser, M. I. & Salh, B. Fecal calprotectin use in inflammatory bowel disease and beyond: A mini -review. Can J Gastroenterol Hepatol 29,157-163 (2015).
4. Mowat, C. et al. Faecal haemoglobin and faecal calprotectin as indicators of bowel disease in patients presenting to primary care with bowel symptoms. Gut gutjnI-2015-309579 (2015). doi:10.1136/gut- jn1-2015-309579.
5. Sherwood, R. A. Faecal markers of gastrointestinal inflammation. Journal of Clinical Pathology 65, 981-985 (2012).
6. Faecal calprotectin diagnostic tests for inflammatory diseases of the bowel I Guidance and guidelines I NICE. Available at: https://www.nice.org.uk/guid-ance/dg11/chapter/6-Considerations.
FECAL ELASTASE
A major cause of chronic diarrhea is Pancreatic Exocrine Insufficiency (PEI) which is a reduction in pancreatic enzyme activity in the intestinal lumen to a level that is below the threshold required to maintain normal digestion. The correct diagnosis and treatment of this condition is very crucial. The Fecal Elastase test is a very sensitive and reliable test that can be used for the diagnosis of PEI.
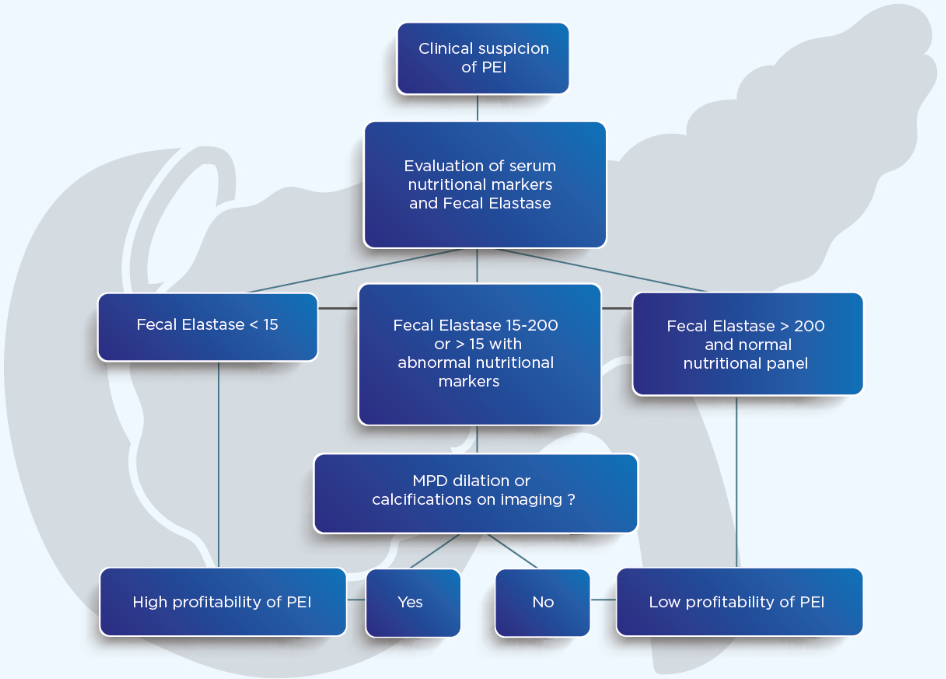
Use of Fecal Elastase and the testing protocol as per suggestions by the British Society of Gastroenterology is depicted below:
References:
1.Luth, S. et al. Fecal Elastase-1 determination: ‘Gold standard’ of indirect pancreatic function tests? Scand. J. Gastroenterol. 36, 1092-1099 (2001).
2. Thomas, P. D. et al. Guidelines for the Investigation of Chronic Diarrhoea, 2nd edition. Gut52, v1-v15 (2003).
3. Lindkvist, B. Diagnosis and treatment of pancreatic exocrine insufficiency. World Journal of Gastroenterologyl9, 7258 (2013).
Dr Lal PathLabs presents disease specific tests to diagnose Gastrointestinal problems :