Fecal Calprotectin – An Intestine Inflammation Detector
Introduction
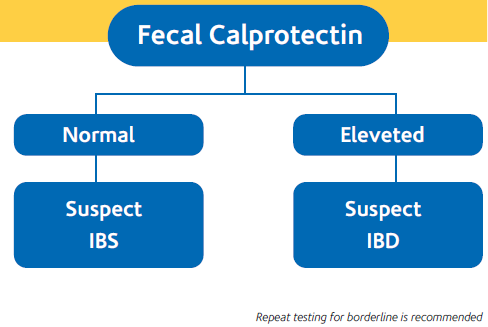
FECAL CALPROTECTIN (FC) is a biochemical test for detection of intestinal inflammation, including inflammatory bowel disease. Fecal Calprotectin testing is recommended as an option to support clinicians with the differential diagnosis of inflammatory bowel disease (IBD) or irritable bowel syndrome (IBS) in adults with recent onset lower gastrointestinal symptoms
Calprotectin
- Calprotectin is a protein belonging to the S100 family and occurring in large amounts in neutrophil ranulocytes, where it accounts for 5% of total proteins and 60% of cytoplasm proteins. Smaller amounts of calprotectin has also been detected in monocytes and activated macrophages.
- The structure of calprotectin consists of a light polypeptide chain and two heavy polypeptide chains, with a molecular weight of 36,5 kDa. Bacteriostatic and mycostatic properties of calprotectin are comparable to those of antibiotics. For this reason the abundance of calprotectin in neutrophil granulocytes and its antimicrobial activity suggest a substantial role in the defence of the organism.
- Calprotectin has been found in several human biological materials: serum, saliva, cerebrospinal fluid and urine. However, the assessment of faecal calprotectin is a widely used method for the detection of bowel inflammation severity. Calprotectin is an extremely stable protein, and it can be found unaltered in stool for longer than 7 days.
- When inflammatory processes occur, calprotectin is released due to the degranulation of neutrophil granulocytes. In bowel inflammation, calprotectin may be detected in the stool. The faecal assay provides direct information about the inflammation site, whereas with serum or plasma, inflammation might be located anywhere.
- An increased Calprotectin concentration in stool is the direct consequence of neutrophil degranulation due to mucosal damage.
Specific indications for measuring fecal calprotectin
NICE (National Institute for Health and Care Excellence) diagnostics guidance [DG11] Oct 2013 recommends its usage for distinguishing organic bowel diseases like inflammatory bowel disease (IBD) from functional bowel syndrome like irritable bowel syndrome (IBS) in adults with recent onset lower gastrointestinal symptoms.
- Assessing efficacy of IBD treatments
- Predicting relapses or flares of IBD
- Offer an alternate diagnostic test for patients who are phobic to invasive procedure or endoscopy
Incidences
- The incidence of ulcerative colitis is approximately 10–20 per 100,000 per year, with a reported prevalence of 100–200 per 100,000 people
- The incidence of Crohn’s disease is around 5–10 per 100,000 per year (and thought to be increasing), with prevalence of 50–100 per 100,000 people
- Prevalence of irritable bowel syndrome in adults varies between 10% and 20% in the general population. Prevalence figures can vary depending on the diagnostic criteria used.
What symptoms would suggest to assay Calprotectin in stool ?
Symptoms suggesting an inflammatory bowel disease (IBD), Ulcerative Colitis and Crohn’s Disease. The mostly common symptoms are as follows:
- recurrent diarrhoea, regardless the amount and/or the presence of blood
- presence of mucus in stool
- diarrhoea often presenting with even severe abdominal pains (in some cases may be mistaken as appendicitis)
- in few cases, fever and weight loss caused by decrease in appetite or malabsorption (decrease of 10-15 kg may occur in a short time)
Irritable bowel syndrome (IBS) & inflammatory bowel disease (IBD)
IBD is the term normally given to a group of conditions that involves inflammation of the gastrointestinal tract, such as Crohn’s disease and ulcerative colitis. These conditions can sometimes have serious complications, including a high risk of surgery and an increased risk of colorectal cancer. In both ulcerative colitis and Crohn’s disease, some people have active disease but no symptoms.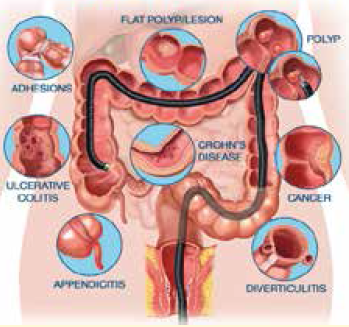 Irritable bowel syndrome (IBS) & inflammatory bowel disease (IBD)
Irritable bowel syndrome (IBS) & inflammatory bowel disease (IBD)
IBS is a functional bowel disorder characterized by frequent bouts of bowel disturbance, abdominal pain and discomfort, and bloating. There is no clear cause, no distinctive pathology and treatment is symptomatic. Exacerbations may be triggered by diet or stress.
Why distinction is required between IBS from IBD?
- Chronic abdominal pain or discomfort, with Diarrhoea or constipation, are common symptoms caused by several different conditions, including Inflammatory Bowel Disease (ulcerative colitis and Crohn’s disease) and IBS (Irritable Bowel Syndrome).
- IBD is the term normally given to a group of conditions that involves inflammation of the gastrointestinal tract, such as Crohn’s disease and ulcerative colitis.
- These conditions can sometimes have serious complications, including a high risk of surgery and an increased risk of colorectal cancer. Patients with IBD need to be referred to specialist care (most likely, gastroenterology) for further investigation.
- IBS is a functional bowel disorder, there is no clear cause, no distinctive pathology and treatment is symptomatic. It is troublesome and can interfere with activities of daily life, although it does not usually cause serious morbidity.
What advantages does Calprotectin offer ?
Calprotectin assay in stool offers significant advantages in the evaluation of intestinal inflammation . In IBD patients level of Calprotectin is very high, while in IBS patients Calprotectin level is higher than in healthy patients but definitively lower than concentration found in active IBD patients.
The senstivity of the assay is 95% with specificity of 93%.
How often Calprotectin can be used in the follow-up IBD patients?
The follow-up of IBD patients subjected to drug treatment is carried out according to criteria that may vary depending upon the status of the patient, response to treatment and clinical remission. Under average conditions, Calprotectin assay should be done 2-3 times/year to check the trend of the faecal Calprotectin concentration. The decrease of Calprotectin values down to normal levels in a short period of time is usually an indication of a better prognosis.
Pediatric and neonatal use
The high sensitivity and specificity of calprotectin make the assay more reliable than other biochemical markers usually used for detecting possible bowel inflammation. In newborns, since bowel function is not yet fully developed, breast or formula feeding during the very first days of life triggers an inflammatory response accompanied by extremely high levels of calprotectin.
In subsequent days, these values decrease when the mucosa recovers its normal functions. Low or absent calprotectin level in newborns might be due to other bowel pathologies and require further investigations.
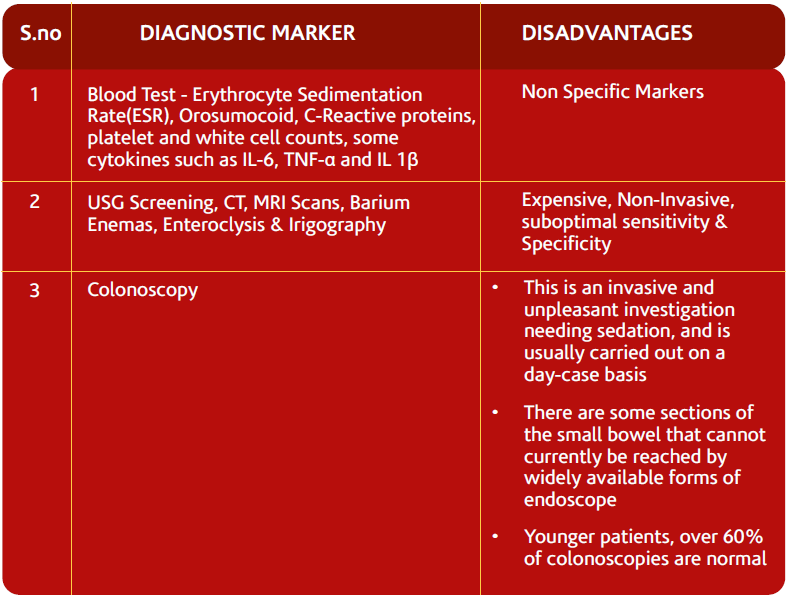
Current diagnostic markers for Inflamatory Bowel Disease
Conclusions
- It is important to distinguish IBD from non-IBD, such as IBS, so that the conditions can be appropriately managed and monitored.
- Fecal Calprotectin offers reliable alternative overcoming these disadvantages and is a easy way to distinguish IBD from IBS.
 Summary & furture presprectives
Summary & furture presprectives
Role of FC has been largely studied in the last years. A good diagnostic precision in discriminating IBD and functional intestinal diseases has been widely reported, thus leading to propose FC as a filter to avoid unnecessary procedures in patients who are most likely to need endoscopy for suspected IBD. FCCs better correlate with IBD activity (more in UC than in CD patients) than the other classically recommended inflammatory parameters (ESR, CRP). FC appears to have a good diagnostic precision in predicting IBD relapse, possibly more in UC than in CD, as well as, more in ileocolonic and colonic than in ileal disease.
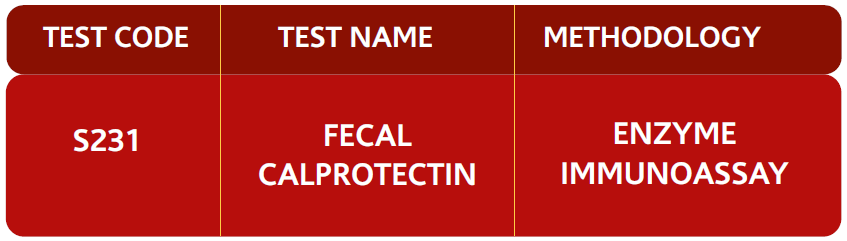
Test range available:
References
- Faecal calprotectin diagnostic tests for inflammatory diseases of the bowel. Issued: October 2013 NICE diagnostics guidance 11, www.nice.org.uk/dg11
- Vermeire S, Van Assche G, Rutgeerts P (2006) Laboratory markers in IBD: useful, magic, or unnecessary toys? Gut 55: 426-431.
- Kopylov U, Rosenfeld G, Bressler B, Seidman E (2014) Clinical utility of fecal biomarkers for the diagnosis and management of inflammatory bowel disease. Inflamm Bowel Dis 20: 742-756.
- Schoepfer AM, Beglinger C, Straumann A, Trummler M, Renzulli P, et al. (2009) Ulcerative colitis: correlation of the Rachmilewitz endoscopic activity index with fecal calprotectin, clinical activity, C-reactive protein, and blood leukocytes. Inflamm Bowel Dis 15: 1851-1858.
- Ho GT, Lee HM, Brydon G, Ting T, Hare N, et al. (2009) Fecal calprotectin predicts the clinical course of acute severe ulcerative colitis. Am J Gastroenterol 104: 673-678.
- Costa F, Mumolo MG, Ceccarelli L, Bellini M, Romano MR, et al. (2005) Calprotectin is a stronger predictive marker of relapse in ulcerative colitis than in Crohn’s disease. Gut 54: 364-368.
- Sutherland AD, Gearry RB, Frizelle FA (2008) Review of fecal biomarkers in inflammatory bowel disease. Dis Colon Rectum 51: 1283-1291.
- Schoepfer AM, Trummler M, Seeholzer P, Seibold-Schmid B, Seibold F (2008) Discriminating IBD from IBS: comparison of the test performance of fecal markers, blood leukocytes, CRP, and IBD antibodies. Inflamm Bowel Dis 14: 32-39.
- Gisbert JP, McNicholl AG (2009) Questions and answers on the role of faecal calprotectin as a biological marker in inflammatory bowel disease. Dig Liver Dis 41: 56-66.
- Korndörfer IP, Brueckner F, Skerra A (2007) The crystal structure of the human (S100A8/S100A9)2 heterotetramer, calprotectin, illustrates how conformational changes of interacting alpha-helices can determine specific association of two EF-hand proteins. J Mol Biol 370: 887-898.
- Vogl T, Gharibyan AL, Morozova-Roche LA (2012) Pro-Inflammatory S100A8 and S100A9 Proteins: Self-Assembly into Multifunctional Native and Amyloid Complexes. Int J Mol Sci 13: 2893-2917.
 National Customer Care : Tel: 011-3988-5050
National Customer Care : Tel: 011-3988-5050
Corporate Office: 12th Floor, Tower B, SAS Tower, Medicity,
Sec- 38, Gurgaon- 122 001, Haryana
Tel: 0124- 3016 500 | Fax: 0124- 42344668
National Reference Lab: Sector-18, Block-E, Rohini, New Delhi- 110 085
www.lalpathlabs.com
doctorfeedback@lalpathlabs.com
Please follow us at : http://www.twitter.com/lalpathlabs : http://www.facebook.com/lalpathlabs