He4 and Risk for Ovarian Cancer Algorithm
He4 and Risk for Ovarian Malignancy Algorithm (ROMA) as New Diagnostic and Prognostic Tools for Epithelial Ovarian Cancer Management
Ovarian cancer (OC) is one of the most deadly gynecological cancers in women. In 2011, there were over 200,000 new cases diagnosed worldwide and 125,000 deaths [1]. The risk of developing ovarian cancer increases with age and most ovarian cancer cases occur in women over 50 years old. Diagnosing ovarian cancer can be difficult
because the symptoms are non-specific and include abdominal fullness, pelvic pain, gastrointestinal distress or fatigue. Over 70% of ovarian cancers are diagnosed at an advanced stage.
Suspected ovarian neoplasm is a common problem in women of all ages. Women have 5 to 10 percent risk of requiring surgery and those who undergo surgery have 13 to 21 percent chance of being diagnosed with ovarian cancer. Since 1980s, CA125 has been utilized in the management of this cancer. Most oncology societies recommend the use of CA125 for the differential diagnosis of a suspected pelvic mass, monitoring efficacy of treatment, and detection of recurrence of ovarian cancer but none of the oncology societies recommend using CA125 for screening for ovarian cancer because CA125 does not have the sensitivity and specificity needed for widespread screening of women.
Human Epididymis Protein 4 (HE 4), has been extensively evaluated and is currently cleared by the Food and Drug Administration (FDA) to be used as an aid in monitoring recurrence or disease progression in patients with ovarian epithelial cancer. HE4 is also used with CA125 in an algorithm called Risk for Ovarian Malignancy Algorithm (ROMA). ROMA has been cleared by FDA as an aid in assessing whether a premenopausal or post menopausal women who presents with an ovarian adnexal mass is at high or low likelihood of being malignant upon surgery. Such improvement would allow for a more accurate presurgical assessment of a woman with a pelvic mass and would facilitate referral of truly high risk women to surgical oncologist and cancer centre for better outcome.
Ovarian Cancer Facts
Ovarian Epithelial cancer (OEC) is the most frequent cause of death from gynecologic cancer. In most of the population based cancer registers in India, Ovarian cancer is the third leading site of cancer among women, trailing behind cervix and breast cancer. The age adjusted incidence rates of ovarian cancer varybetween 5.4 to 8.0 per 100,000 populations in different parts of the country [2].
Ovarian cancer is a relatively manageable malignancy when diagnosed at an early stage, but late stage detection almost always translates into poor prognosis.Early detection of ovarian cancer corresponds to a 92% five years survival rate where as overall 5 year survival rate for ovarian cancer is less than 50%. This is because only
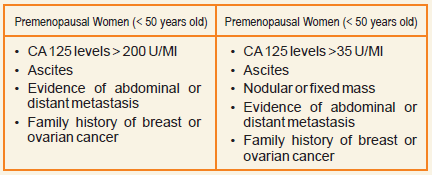
19% of ovarian malignancies are diagnosed prior to extra-ovarian spread owing to the lack of obvious symptoms prior to progression [3].Ovarian cancer survival rates could be improved through screening and early detection. Disappointingly, effective screening methods have not been established and continue to be elusive. Equally important recent studies have demonstrated that women who have their initial surgery performed by gynecologic oncologist and at centers having experience in the treatment of ovarian cancer have better survival rates [4]. The improved survival rate is result of proper staging which helps identify patients with unexpected occult metastasis who need adjuvant therapy, and of aggressive debulking of advanced disease. Thus in women presenting with an adnexal mass, clinicians must assess the malignant potential of the pelvic mass in order to best determine the optimal location and clinician to provide initial intervention.The American College of Obstetricians and gynecologists (ACOG) in conjunction with the Society of gynecologic Oncologists (SGO) published referral guidelines in 2007 to provide guidance on the management ofadnexal masses (Table 1).
Table 1. ACOG and SGO Referral guidelines for a Newly diagnosed Pelvic Mass
Dearking et al (15)evaluated these guidelines in a large cohort of women and found that these guidelines exhibited a positive predictive value (PPV) of 64.6% in postmenopausal women and 39.6% in premenopausal women. Theguidelines generally worked well in postmenopausal women, but performedpoorly in early-stage disease, especially among premenopausal women.
Thus an effective differentiation approach is still needed that will help differentiate benign lesions from malignant lesions and would allow referral of high risk women to specialized center that would improve clinical outcomes.
Evaluation of Adnexal Mass
Premenopausal Women (< 50 years old) Postmenopausal Women (> 50 years old)
- Physical examination: Physical examination have limited ability to identify adnexal masses, especially in patients whose body mass index is greater than 30 kg per m2.
- Ultrasonography: High frequency, grey scale transvaginal ultrasonography (USG) can produce high resolution images ofadnexal mass and is the only one recommended for routine use. Color Doppler USG measures blood flow indices; however, its use is controversial because the values of these indices overlap considerably between benign and malignant masses. CT, MRI & PET should be used in special circumstances because of high cost.
- Serum marker screening: CA 125 antigen is the most extensively studied serum marker for distinguishing benign from malignant pelvic masses. CA 125 is elevated in 80 percent of patients with OEC and has been show to correlate with tumor volume and stage making it an excellent marker for monitoring response to therapy. However, it is elevated only in 50 percent patients with stage I disease. For this reason, measurement of CA 125 in not a useful screening test. CA 125 specificity is also compromised by the fact that many benign gynecologic and medical conditions as well as other malignancies can result in elevated CA 125 levels.
Several other serum tumor markers have been evaluated in combination with CA 125 to improve the sensitivity, specificity and positive predictive value of the test. Moore et. al. (6) evaluated several candidate biomarkers and found that combination of CA 125 and HE4 gave the best sensitivity and specificity of all biomarkers tested in women presenting with pelvic mass. Nolen and colleagues found that combination of CA125 & HE4 had the best discriminatory power for benign versus malignant disease than all other malignancies. Yurkovetsky and colleagues found that a combination of CA125, HE4, Carcinoembrynic antigen and Vascular cell adhesion molecule 1 gave the best sensitivity of all the combinations tested. Currently there are many groups that are evaluating HE4 in combination with CA125, or in combination with other biomarkers.
Human Epididymis protein 4 (He4)
He4 is a glycoprotein that is expressed in normal male and female reproductive tract and pulmonary epithelium. The gene encoding for HE4 is part of a family of protease inhibitors involved in protective immunity in ovarian malignancies as well as endometrial cancer (EC). Moore et al upon testing the efficacy of various markers of OC demonstrated that as a single maker, HE4 had the highest sensitivity of 72.9% at a set specificity of 95%. The combination of CA125 with HE4 achieved the highest sensitivity (76.4%) compared with all other single marker or dual marker combinations, and the addition of other markers to combination of HE4 & CA125 imposed only modest improvement in sensitivity of OC detection. Havrilesky and colleagues obtained similar results in an independent study of another group of OC markers. These studies demonstrate that as individual tests CA125 & HE4 have equivalent sensitivities for detecting malignancy in a woman presenting with pelvic mass, but in combination the tests could be complementary.
In contrast to CA 125, HE4 is usually not elevated in benign gynecologic conditions such as non malignant tumors, endometriosis and pelvic inflammatory disease.Huhtinen and colleagues recently analyzed serum concentration of CA125 in 225 women with OC, EC, endometriosis or healthy controls. The combination of HE4 and CA125 achieved much improved sensitivity of 92.9% at 95% specificity compared with either HE4 or CA125 alone. HE4 levels were elevated in both OC and EC, but not in endometriotic lesions.
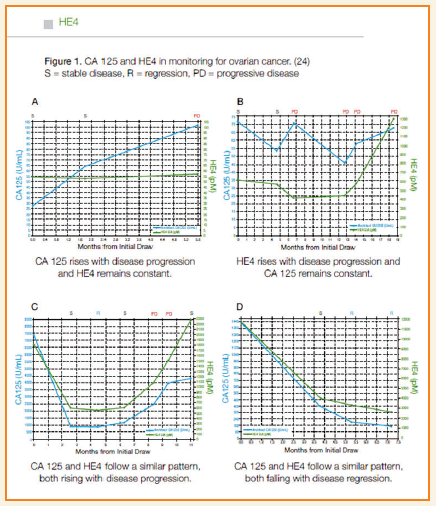
HE4 has been cleared by the FDA for monitoring recurrence in patients with OEC. Allard et al showed that HE4 demonstrated a 76.2% overall concordance with disease progression or regression, and in some cases, HE4 is elevated where CA 125 is not. CA125 is the most commonly used marker for monitoring treatment of OEC, but some 10% of patients of OC may not have elevated levels of CA125 and these patients are therefore left without a reliable marker for monitoring of disease.Recently, the novel biomarker HE4 has been shown to elevated in over half of OEC patients where CA125 was not elevated resulting in over 90% of patients having at least CA125 or HE4 as a biomarker for monitoring disease. However, most studies with HE4 have focused on its potential ability to differentiate benign from malignant lesion in women presenting with an adnexal or pelvic mass.
ROMA :
Even in combination serum biomarkers have limited sensitivities and specificities, so efforts to improve risk stratification tools for women with pelvis masses have incorporated other factors from woman’s clinical evaluation. Moore and colleagues developed an algorithm incorporating CA 125, HE4 and menopausal status, called Risk for Ovarian malignancy Algorithm (ROMA) which has been cleared by FDA as an aid in assessing whether a premenopausal or postmenopausal women who presents with an ovarian adnexal mass is at high or low likelihood of finding malignancy upon surgery.
ROMA uses the results for HE4 and CA125 to generate apredictive index (PI) for OEC calculated by thefollowing formulas:
For premenopausal women:
PI = -12.0 +2.38 *ln(HE4) + 0.0626 *ln(CA125)
For postmenopausal women:
PI = -8.09 +1.04 *ln(HE4) +0.732 *ln(CA125)
Then, ROMA value is calculated as follows:
ROMAvalue (%)= exp(PI)/[1 +exp(PI)] *100
According to the indications of the HE4 manufacturer,indexes of at least 7.4% and 25.3% indicate a highrisk for the presence of EOC in pre- or postmenopause, respectively.
Moore et al. reported that ROMA successfully classified women presenting with a pelvic mass into low and high risk groups with 93.8% of women who were found to have OEC to be correctly identified as high risk. Most recently, Moore and Colleagues compared ROMA to the Risk of Malignancy Index (RMI)that is comprised of the measurement of CA 125 levels in addition to an imaging score and assessment of menopausal status to predict OEC women presenting for surgery with a pelvic mass. At a set specificity of 75% ROMA demonstrated a sensitivity of 89% compared to 80.7% of RMI, a difference which was statistically significant (p=0.0113).
A recent metaanalysis [7] found that, first, ROMA could help distinguish OEC from benign pelvic mass with a high diagnostic accuracy (AUC: 0.93). The ROMA has high sensitivity to predict advanced stage OEC than early stage OEC and in postmenopausal women than in premenopausal women. Second, although HE4 has higher specificity than CA125 for OEC monitoring, CA125 has better diagnosis accuracy (higher AUC) than HE4 for OEC or OC prediction. This is based on the results of 4 studies that compare HE4 and CA125 within the same population. Third, based on the results of comparison of HE4, CA125 and ROMA in the same population, the overall performance (AUC) of the three tests for OEC prediction are similar. ROMA inherits the strengths and weakness of CA 125 and HE4 alone. Indeed, ROMA is more sensitive than HE4 but less sensitive that CA 125 and it is more specific than CA 125 but less specific than HE4.
Key points:
- Ovarian epithelial cancer (OEC) is the deadliest of the gynecological cancers with the majority of patients diagnosed at an advanced stage.
- Patients with OEC show improved outcomes when surgery is performed by an experienced gynecological surgeon or at experienced OEC treatment centers.
- Currently CA 125 is the biomarker that is used to aid in the management of OEC patients but the marker has limited sensitivity and specificity.
- HE4 is a new biomarker for OEC and has been approved by FDAin monitoring recurrence or progression in OEC patients.
- HE4 is also used with CA 125 in an algorithm called Risk of Ovarian Malignancy Algorithm (ROMA).
- ROMA is an aid in assessing the risk of malignancy upon surgery in womenwho present with an ovarian adnexal mass,patients at high risk can have their surgeryperformed by an experienced gynecological surgeon or at an experiencedOEC treatment center for better outcome.
Dr. Nimmi Kansal, MD
HOD, Biochemistry & Immunoassay
National Reference Laboratory
Dr. Lal PathLabs
Bibliography :
- SGO White Paper On Ovarian Cancer: Etiology, Screening And Surveillance. GynecolOncol 2010;119:7-17
- Consolidated Report of Population Based Cancer Registries 2001-2004. National Cancer Registry Program. Indian Council of Medical Research Banglore : 2006
- HE4 As A Biomarker For Ovarian And Endometrial Cancer Management. Expert Rev MolDiagn 9(6);200:555-566
- The Outcomes of Ovarian Cancer Treatment Are Better When Provided By Gynecologic Oncologists And In Specialized Hospitals: A Systematic Review. GynecolOncol 2007;105:801-12.
- Practice Guidelines: ACOG Releases Guidelines on Management Of Adnexal Masses. Am Fam Physician 2008; May; 77(9):1320-1323.
- Moore RG, Brown AK, Miller MC, et. al. The Use of Multiple NovelTumor Biomarkers For Detection of Ovarian Carcinoma in Patients With A Pelvic Mass. GynecolOncol 2008;108:402-8.
- Does Risk For Ovarian Malignancy Algorithm Excel Human Epididymis Protein 4 And CA125 In Predicting Epithelial Ovarian Cancer: A Meta-Analysis.BMC Cancer 2012, 12:258
Feel the anxiety of a woman with an ovarian cyst detected during a routine checkup. Add to this her apprehension of what might be discovered at surgery. Bundle this with the challenge you face to accurately identify – before initial surgery – whether the mass is most likely to be benign or malignant. What you have at hand here is a good reason to measure HE4 in your patients who have a pelvic mass or a complex ovarian cyst.
Determining the presence of malignancy is a major goal in the preoperative evaluation of a woman who has a pelvic mass. As noted in various studies, referring a patient in whom you suspect ovarian cancer to a specialty center for surgery / care increases her chances for survival.
Measuring HE4 and CA125 in combination may represent a significant advance in our ability to accurately identify and triage patients who are at high risk of serous or papillary ovarian cancer.
A major hurdle towards reducing mortality continues to be the late presentation of the disease. Less than a third of women are diagnosed with early-stage disease, for which survival at 5 years is 90%—indicating that early diagnosis and treatment is central to reducing mortality.
Ovarian cancer: breaking the silence – Ovarian cancer has often been called a silent killer because of its subtle and non-specific symptoms; however, it is perhaps not so much that the disease is silent, but rather that it is not being heard. Early OC detection corresponds to a 92% 5-year survival rate, whereas the overall 5-year survival rate for ovarian cancer is less than 50%. This is because only 19% of ovarian malignancies are diagnosed prior to extra-ovarian spread owing to the lack of obvious symptoms prior to progression
Major advances into breaking the silence are long overdue. A noninvasive means of discriminating between malignant pelvic masses and benign lesions is important given that approximately 20% of women will develop an ovarian cyst or pelvic mass at some point in their lives. Without adequate means of discerning the malignant potential of these tumors, a considerable proportion of these women will have unnecessary surgery.
In this issue of ‘Insight’, Dr Nimmi Kansal details how HE4 is a novel biomarker which allows disease stratification, monitoring of response to therapy, and surveillance for post-surgical recurrence in women with a diagnosis of OC.
Compared with screening and personalized therapy, risk stratification and proper triaging could be achieved by using theunique abilities of HE4 and CA-125 in distinguishing patients with ovarian malignancy from those with benign ovarian or endometrial conditions. This could be used to refer patients to centers specializing in ovarian cancer treatment, given that these patients have been shown to have more favorable outcomes.
We may argue that to truly affect the cure of ovarian cancer, we need better diagnostic tools for asymptomatic women. Till then – if you haven’t measured HE4 in your patient with a pelvic mass or a complex ovarian cyst, consider evaluating the utility of this assay in your clinical practice. There is a good reason to do so.
It is indeed encouraging to have received a tremendous response to the previous issue of INSIGHT and we continue to look forward to your valuable feedback and suggestions to guide us in addressing the various issues of diagnostic service. Your participation is vital to help us improve and provide you the best quality information in the field of diagnostics and their application in clinical diagnosis and treatment. We look forward to your participation and continued support.