ANTI-MULLERIAN HORMONE — A MARKER FOR OVARIAN FUNCTION
Introduction
Anti-Mullerian hormone (AMH) is a dimeric glycoprotein, a member of the transforming growth factor beta superfamily which acts on tissue growth and differentiation, AMH was originally identified because of its fundamental role in male sex differentiation. Indeed, expressed in the sertoli cells of the fetal test is and induces regression of the Mullerian ducts. In the absence of AMH mullerian ductevolves into uterus, fallopian tubes and the upper part of vagina.
In women, AMH is produced by granulosa cells from preantral and antral follicles and main physiological role of AMH in ovary appears to be inhibition of the early stages of follicular development. Recently. AMH has been evaluated by several groups as a potential novel clinical maker of ovarian reserve and of response to gonadotropins.
In women, AMH is produced by granulosa cells from preen.] and antral follicles and main physiological role of AMH in ovary appears to be inhibition of the early stages of follicular development. Recently, AMH has been evaluated by several groups as a potential novel clinical maker of ovarian reserve and of response to gonadotropins.
AMH in Ovarian Physiology
AMH is produced by granulosa cells from preantral and antral follicles, AMH is expressed on follicles that have undergone recruitment from primordial follicles pool but have not been selected for dominance by the action of FSH. In human this occurs in antral follicles of size 4-6 mm. AMH is not expressed in primordial follicles, atreticfollicles and theca cells.
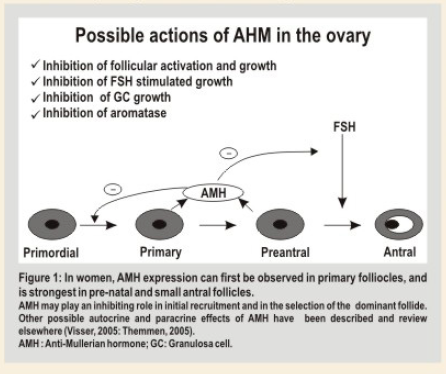
The main physiological role of AMH in ovary seems to be limited to inhibition of the early stages of follicular development (Figure 1). Several studies have confirmed the concept that in the absence of AMH, primordial follicles are recruited at a faster rate, resulting in premature exhaustion of primordial follicle pool. In vitro studies have shown that AMH inhibits FSH dependent follicular growth and regulates ovarian steroidogenesis by decreasing expression of aromatase on granulosa cells thus decreasing estradiol production. AMH reduces LH receptor on granulosa cells stimulated by FSH.
Factors Modulating AIVIH Levels In Women In women
AMH levels are almost undetectable at birth with a subtle increase within first 2 or 4 years of age, after that AMH appears to be stable until adulthood but found to decrease as a sign of follicular reserve exhaustion becoming undetectable at menopause.
AMH levels seem to be unmodified under conditions in which endogenous gonadotropins release is substantially diminished such as during pregnancy, GnRH agonist treatment and short term oral contraceptive administration, indi.ting that non cyclic FSH independent ovarian activity persist, even when pituitary FSH is suppressed.
AMH levels in obese women may be lower for physiological reasons related to obesity itself and may not necessarily indicative of impaired ovarian reserve. Other factors related to reducedAMH levels are smoking, alcohol use and certain race or ethnicity.
AMH in Ovarian Reserve Testing
The ovarian reserve, constituted by the size of ovarian follicles pool and the quality of oocytes therein, declines which increasing age, resulting in the decrease of a woman, reproductive function.
For women who want to become pregnant by means of assisted reproduction technique (ART), it is important to offer counseling about the optimal balance between benefit and risk. Since these out comes are highly dependant on ovarian reserve, much efforts have been put in identifying good clinical markers of ovarian reserve regarding individuals prognosis for success and to design appropriate stimulation protocols.
An ideal ovarian reserve test should permit identification of women who have a chance of pregnancy after IVF close to zero as a consequence of an extremely reduced ovarian reserve. The exclusion of these couples from ART could effectively reduce costs for the health system. Moreover unnecessary medical treatments, stress and disappointment could be avoided. The possible aims of ovarian reserve testing in the IVF setting are:
i. Tocounsel the patients about the risk benefit for treatment.
ii. To reduce the cost by denying treatment to bad prognosis couples.
iii. To individualize treatment strategy.
To assess an individual’s ovarian reserve, early follicular phase serum levels of FSH, inhibin B and estradiol (E2) have been measured. Inhibin B and E2 are produced by early antral follicles in response to FSH, and contribute to classical feedback loop of the pituitary•gonadal axis to suppress FSH secretion. With the decline of follicle pool, serum level of inhibin B & E2 decreases & subsequently FSH rises. Because these factors are part of a feedback system, their levels are not independent of each other. Furthermore changes in serum level of FSH, inhibin B and E2 occurs late in reproductive ageing process. So far, assessment of number of antral follicles by USG, the antral follicles counts (AFC) best predicts the quantitative aspect of ovarian reserve. However, AFC at times is technically challenging and highly operator dependent. Therefore, a serum marker that reflects the number of follicles that have made the transition from the primordial pool into growing follicle pool, and that is not controlled by gonadotropins, would benefit both patients & clinicians.
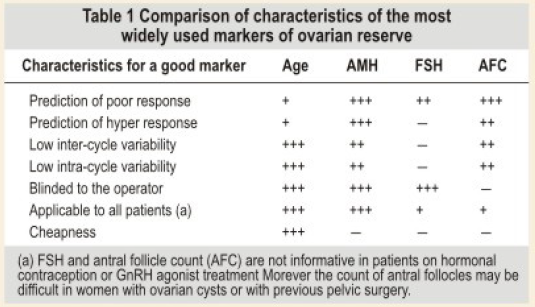
Recently, AMH has been proposed as an ideal test for ovarian reserve testing (Table 1) due to the following characteristics:
1. Decreases continually during the fertile life.
2. Not influenced bygonadotropin feedback mechanism.
3. AMH level shows very low inter and intracycle variability thus can be measured independent of the day of cycle.
4. Bestcorrelating marker withAFC.
Significance of lowAMH levels before IVF
For women with low AMH levels either cycle cancellation or poor response may be anticipated. Her. couple need to accept protract. treatment programs and should be inform. that not every cycle may result in embryo transfer and that it is highly probable that chance of suc.ss may be reduced. Cut -off values of 0.7 — 0.75 ng/ml has been proposed by several groups for the identificetion of poor responders, by this cut off 75% of poor responder are correctly identified.
Significance of NormalAMH levels before IVF:
Wornen with normal AMH levels are most probably normal responders and good prognosis may be anticipated.
Significance of high AMH levels before IVF:
Women with high AMH levels are considered to be at risk for hyperresponse and OHSS. Hence these wornen should be informed about the risk and may really benefit from individualization of the treatment. Indeed a low FSH starting dose followed by the use of GnRH antagonists have been shown to reduce the incidence of OHSS.
AMH AS A MARKER OF OVARIAN AGING
Quantitative aspect of ovarian aging is reflected by a decline in size of the primordial follicle pool. Direct measurement of this pool is impossible. However, the number of Primordial follicles is directly reflected by number of growing follicles. Sin. AMH is secreted by growing follicles up to selection, it seerns to be a promising cendidate. Moreover changes in AMH levels occur relatively early in the sequence of events associated with ovarian aging. Substantially elevated serum levels of FSH are not found until cycles have become irregular. Therefore, a marker that already shows a considerable change when cyclicity is still norrnal would better identify women with declining fertility.
Measurement of AMH to assess ovarian age may be of considerable interest for wornen in general since a considerable proportion of subferility is due to postponement of child bearing. Measurement of ovarian reserve may provide insight into the number of fertile year’s women has left.
AMH as A Marker for Ovarian Pathophysiology
Besides being a marker for diminishing follicle pool serum AMH level cen a. serve as a marker in ovarian pathophysiology, such as polycystic ovary syndrome (PCOS), in which the antral follicle pool is enlarged. In PCOS women, the Iwo to threefold increase in number of growing follicles is reflected by two to three fold increases in serum AMH level. In PCOS, follicular excess is mainly ceused by an increase in small antral follicles up to 2-5 mm size. Interestingly, in follicles beyond this stage AMH expression decreases. Therefore, it is not surprising that serum AMH levels positively correlate with number of 2-5 mm, but not 6-9 mm follicles in PCOS women. The finding thatAMH level is also increased in the follicular fluid of PCOS women suggests that an increase in serum AMH may also result from increased AMH production per follicle. Some of the studies have indicated that PCOS women reach menopause atan older age. The ovarian ageing process in PCOS women may have been slowed down. possibly due to suppre.ed prirnordial follicle outgrowth by the high levels of AMH observed in the. women. AMH levels appear to be related to severity of the syndrome since levels have been observ. to be higher in insulin resistant PCOS women than in patients with normal insulin sensitivity. Similarly AMH is higher in amenorrheic compared with oligomenorrheicwomen with PCOS.
Conclusion
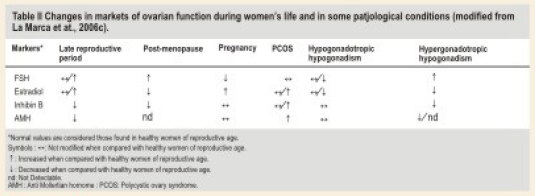
The currently available data indicate that serum AMH levels decrease with age in premenopausal women. Assessment of ovarian reserve is particularly important in IVF clinic. A serum level of AMH strongly correlates with antral follicle count and reflect the size of primordial follicle pool thus may be useful as a predictor of ovarian responsiveness. The changes in AMH levels in several physiological and pathological conditions are reported in Table 2.
AMH may permit the identification of both the extremes of ovarian stimulation: a possible role for its measurement may be in the individualization of treatment strategies. Furthermore, AMH measurement in combination with other tests of ovarian reserve (antral follicle count, FSH, estradiol and Inhibin B levels) can assist women in making more informed family planning decisions based on their own individual risk of experiencing premature loss of ovarian reserve.
References:
1. A. La Marca, G.Sighinoifi, D. Radi, C. Argento, E. Baraldi, A. Carducci Artenisio, G. Stabile and A. Volpe. Anti Mu Ilerian hormone (AMH) as a predictive marker in assisted reproductive technology (ART). Human Reproduction Update, Vol 16, No.2pp 113-130, 1020.
2. A. La Marca, F.J Broekmans, A Volpe, B.C. fauser, and N.S. Macklon, on behalf of the ESHRE Special Interest Group for Reproductive Endocrinology – AMH Raound Tble Anti-Mu Ilerian hormone (AMH); what do we still need to know? Human Reproduction Vol. 24, No9pp. 2264-2275, 2009
3. Jenny A Visser, Frank H de Jong<, Joop S E Laven and Axel P N Themmen. Anti-Mu Ilerian hormone (AMH); a new marker for ovarian function. Reproduction (2006); 131, 1-9
THE THINPREP PAP TEST — THE NEXT GENERATION OF CERVICAL SCREENING
Introduction
Cervical cancer is the most preventable gynaecological cancer. It is disheartening to note that it is still the seoond most common cancer among women in developing countries with only breast cancer occuMng more commonly. In India this is the commonest cancer among women and this country has the largest burden of cervical cancer patients in the world.
The medical dictum ‘Prevention is better than cure” could not be more appropriate in this situation. The natural history of cervical cancer is such that the cervical cells undergo dysplasia, initially mild, to moderate and then severe before developing into cervical cancer. The rationale of the screening programme is to detect the abnormal cell before it becomes cancerous and treat it appropriately. With the establishment of a successful screening programme, pap tests have been proven to reduce the incidence of cervical cancer and mortality by 50%
India with its highest share of global burden of cervical cancer has to implement a population based cervical cancer control program to reduce the number of deaths. There are new screening options available like visual inspection after acetic acid application (VIA) test, single visit approach A screening and treatment etc. Emergence of the two effective vaccines against human papillornavirus (HPV), the necessary cause of cervical cancer, has introduced a fresh lease of life to the cervical cancer control strategies. A vaccine-based programme is not going to be 100 per cent protective as cervical cancer can still be caused by HPV types not prevented by the vaccines. Girls and women who are already infected by the HPV types 16 and/or 18 are not likely to be benefited by the vaccines. The cost of vaccine is still prohibitively high to consider its introduction in a broad based national program and is a major impediment to implement a vaccine-based primary prevention approach.
Even after introduction the impact of vaccination on the disease burden in the population is going to take 15- 20 years to be evident. During this intervening period cervical cancer screening is the only feasible option to reduce cervical cancer deaths in India .
The Conventional PAP smear
Invasive cancer of the uterine cervix is preventable when its precursor lesions are detected and treated early. Cervical cytology has been in use now for more than 50 years, and has proven itself to be the main weapon of defence against this disease Cervical cytology was introduced by George Papanicolaou into clinical practice in 1940. the conventional Papanicolaou smear involves taking a sample of cells from the cervix and viewing them under a microscope to check for dysplatic cells (abnormal cell changes)
The conventional method involves using a speculum to insert into the vagina and visualize the cervix, a sample of cells is collected from inside and around the cervix using a small brush and spatula. The sample is smeared onto a glass slide and fixed with alcohol to send to the laboratory for screening. The efficacy of a cervical screening method is measured by its ability to diagnose precencerous lesions.
In recent years, the accuracy of the conventional Pap smear has come under a great deal of scrutiny. The false negative rates (the test is negative even though the patient has the disease) of conventional pap smears have been reported to range from 10 to 50%. These are due to the limitations of sampling or slide preparation. Abnormal cells may also go undetected because of poor smear quality. Accurate interpretation can be adversely affected by the Presence Of blood, mucus, obscuring inflammation and air-drying artifact.
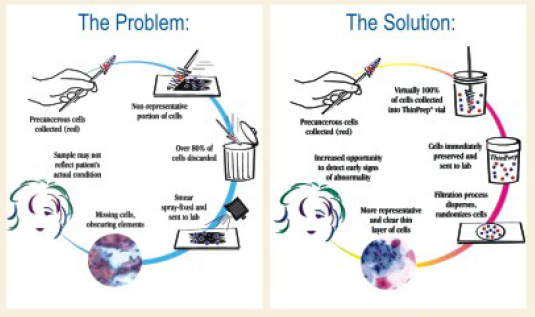
The ThinPrep PAP smear – New technology to address the problems of Conventional PAP smear
To address the problems of false negative rates of conventional pap test, a new liquid-based, thin-prep Pap test has been approved by the US Food and Drug Administration in 1996. With this method, the cervical sample is taken from the patient in the usual manner. Acytobrush is used to collect the sample. However, instead of smearing onto a glass slide, the cells are rinsed into a small vial containing preservative solution. Sample is later processed and screened in the laboratory. Studies have proved that this method to be more sensitive to detect the precancerous lesions than the conventional pap test.
In clinical trials and routine clinical practice, the ThinPrep Pap Test has been shown to be more effective than the conventional Pap smear in several ways including significantly improved detection of low-grade and high-grade intraepithelial lesions, and a significant improvement in specimen adequacy
Conclusion
The ThinPrep PapTest is a significant innovation in the field of cytological testing, given that it is the first evolution to the Papanicolaou Test six decades after it was first introduced to the market, contributing significantly in decreasing the rate of cervical cancer.
It is currently the most widely used method for testing women for cervical cancer considering the following advantages,
1. being significantly more effective than the conventional PapTest for the detection of low and high grade lesions in a variety of patient populations
2. Advanced technology provides significantly improved specimen quality in a variety of patient populations.
3. Approved for use with either broom-type or endocervical brush/spatula collection devices.
4. Simplified Borderline Smear management with HPV testing.
In conclusion, studies of the ThinPrep Pap Test show that this new technology significantly increases the detection of squamous intraepithelial lesions of the cervix – by improving , the quality of the sample and reducing the likelihood of false negative cytology results. it will significantly improve early detection and treatment of cervical abnormalities without dictating a change in screening intervals.
significantly increases the detection of squamous intraepithelial lesions of the cervix – by improving , the quality of the sample and reducing the likelihood of false negative cytology results. it will significantly improve early detection and treatment of cervical abnormalities without dictating a change in screening intervals.

From the Editor’s Desk
 Anti-M011erian hormone (AMH) is a promising marker of ovarian reserve. With the current pace of AMH research, the boundary between interesting research and clinical practice is becoming more defined. Overall, these are particularly exciting times for those working on clinical aspects of AMH and this is clearly a hormone for which a time of recognition has come. In this issue Dr Nimmi Kansal highlights key inflection points in ovarian follicle dynami. and addresses some pertinent questions – What exactly does AMH do? What practical clinical applications exist for the measurement of serumAMH?
Anti-M011erian hormone (AMH) is a promising marker of ovarian reserve. With the current pace of AMH research, the boundary between interesting research and clinical practice is becoming more defined. Overall, these are particularly exciting times for those working on clinical aspects of AMH and this is clearly a hormone for which a time of recognition has come. In this issue Dr Nimmi Kansal highlights key inflection points in ovarian follicle dynami. and addresses some pertinent questions – What exactly does AMH do? What practical clinical applications exist for the measurement of serumAMH?
The burden of cervical cancer in India is enormous, accounting for about 20 per cent of all cancer related deaths in women and is the number one cause of death in middle aged Indian women. It is paradoxical that so many deaths are occu.ng in spite of cervical cancer being a preventable disease. In this issue Dr Hemamalini Aiyer reviews the advantages of the newer technology ThinPrep PAP smear in significantly improving eady detection of moderate to severe dyskaryosis for eady detection and treatment of cervical cancer.
Your appreciative feedback is very encouraging and suggestions are invited to help us improve and provide you the best quality information in the field of diagnostics and their application in clinical diagnosis and treatment.
We look forward to your participation and continued support.
Dr Reena Nakra
Chief Editor,
Head Integration Group, MA labs
E-mail: reena.nakra@lalpathlabs.com