Biochemical Markers of Bone Turnover
BIOCHEMICAL MARKERS OF BONE TURNOVER
With the ageing population in most countries, disorders of bone and mineral metabolism are becoming increasingly relevant to everyday clinical practice. Consequently, the interest in, and the need for effective measures to be used in screening, diagnosis and follow up of such pathologies have markedly grown. Together with clinical and imaging techniques, biochemical tests play an important role in the assessment and differential diagnosis of metabolic bone diseases. These biochemical markers are non-invasive, comparatively inexpensive when applied correctly, helpful tools in the diagnostic and therapeutic assessment of metabolic bone diseases.
Bone is constantly undergoing a metabolic process called remodeling. This includes a degradation process, bone resorption, mediated by the action of osteoclasts, and a building process, bone formation, mediated by the action of osteoclasts. Remodeling is required for the maintenance and overall health of bone and is tightly coupled; that is, resorption and formation is in balance. In abnormal state of bone metabolism, this process becomes uncoupled and when resorption, exceeds formation, this result in a net loss of bone.
Osteoporosis is a metabolic bone disease characteristics by abnormal bone remodeling. It is systematic skeletal disease characterized by low bone mass and microarchitechtural deterioration of bone tissue with a consequent increase in susceptibility of fractures. The most common type of osteoporosis occurs in post-menopausal women as a result of estrogen deficiency produced by the cession of ovarian function. Restoration of premenopausal estrogen levels by replacement therapy prevents bone loss and osteoporosis. Osteoporosis can also results from an inadequate peak boke mass during the growing years, an aged related imbalance of bone remodeling with not excess of resorption and a number of clinical conditions and therapies that induce bone loss or bone remodeling imbalances. These include endocrine diseases such as hypogonadism, hyperthyroidism, and hypercorticolism; gastrointestinal diseases related to nutrition and mineral metabolism; connective tissue disease; multiple myeloma; chronic immobilization, alcoholism, and chronic therapy with heparin or corticosteroidsd. Other diseases characterized by bone remodeling include Paget’s disease and metastasis to bone.
Bone turnover markers, are indicators of bone metabolism derived from bone matric or bone cells. They are important diagnostic aid in the evaluation and management of osteoporosis. Bone markers allow for efficient therapy monitoring and compliance testing of osteoporotic patients. They can also help in fracture risk prediction. The international osteoporosis foundation (IOF) supports the use of bone markers with published guidelines.
Markers of Bone Formation:
Bone formation markers are products of osteoblast expressed during different phase of osteoblast development. They are considered to reflect different aspects of osteoblast function and of bone formation. All markers of bone formation are measured in serum or plasma.
- Bone alkaline phosphatase
The activity of bone ALP is elevated with increased osteoblast activity such as in Paget’s disease, high turnover osteoporosis, hyperparathyroidism, osteomalacia and rickets etc. Advantages of using the marker
- Long halflife if 1 to 2 days in serum
- Unaffected by diurnal variation
- Not affected by declining GFR, thus more useful than osteocalcin in impaired renal function
- Highly sensitive & specific marker for diagnosis of Paget’s disease.
Bone APL is not a reliable marker in liver disease and in patients with abnormal level of 1,25 dihydroxy vitamin D.
- Osteocalcin
Osteocalcin is synthesized in the skeleton by osteoblasts the cells responsible for bone formation. Its synthesis is stimulated by 1,25 dihydroxyvitamin D and it is rapidly cleared by kidney, thus has a short half life. It is highly sensitive and specific maker of bone formation. Its levels are increased in hyperparathyroidism, Paget’s disease, high turnover osteoporosis hyperthyroidism, renal osteodystrophy, fracture, and acromegaly and are decreased in hyperparathyroidism. Growth hormone deficiency, during estrogen replacement therapy, during treatment of glucocorticoid, bisphosphonates, and calcitonin. Osteocalcin may be misleading in certain situations as it may be elevated in patients of renal failure and in patients on treatment of Vitamin D.
- Procollagen Peptides
Another test for assessing bone formation or osteoblastic collagen synthesis is determination of propeptides of type I collagen. Type I collagen is the most abundant collagen found in bone. It is also found in other tissues such as skin, dentin, cornea, vessels etc. and tendons in bone; collagen is synthesized as pre-procollagen containing both N and C terminal extensions. These extensions or propeptides are cleared from Type I collagen during fiber formation and circulate in blood. Assays are available both for the amino (N-) propeptide (P1NP) and the carboxy (C-) terminal propeptide (P1CP). But clinical relevance of P1CP is still in evaluation and serum P1CP appears to be of greater diagnostic validity. From practical point of view thermostability of P1NP is an advantage in that extended transport and storage times are well tolerated without significant loss of activity. Measurement of P1NP is helpful for assessing bone formation in patients treated with vitamin D or in patients with abnormal level of these hormones where osteocalcin and bone alkaline phosphatase may be misleading.
Markers of Bone Resorption
Marker of bone resorption include collagen cross links such as pyridinolines and N and C telopeptides, acid phosphatase, urinary galactosyl hydroxylysine and urinary hydroxyproline.
- Puridnolines (Deoxypyridinoline (DPD) and pyridinoline (PYD)
PYD and DPD are formed during the extracellular maturation of fibrillary collagens. They bridge several collagen peptides and mechanically stabilize the collagen molecule. During bone resorption, crosslinked collagens are proteolytically broken down and these cross linked components are released into circulation and urine. DPD is sound in significant amount in bone, ligaments and arota. DPD appears to be specific and sensitive markers of bone resorption for several reasons:
- It is formed during collagen maturation and nor during biosynthesis. Thus originates only as degeneration product of mature matrix.
- It does not appear to be metabolized prior to excretion in urine
- Bone is the major source of DPD
- DPD does not appear to be absorbed from the diet.
Thus, pyridinium cross links are currently viewed as the best indices for assessing bone resorption.
- Cross Linked telopeptides of Type I collagen
The cross linked telopeptides of type I collagen are derived from specific region of the collagen type I molecule, namely aminoterminal telopeptide (NTP) and Carboxy terminal (CTP) telopeptide.
Elevated levels of pyridinolined and telopeptides have been reported in osteoporosis, Paget’s Disease, metastic bone disease, primary and secondary hyperthyroidism, and other disease with increased bone resorption. When postmenopausal women are compared with premenopausal controls, telopeptides are usually are increased more than other markers of resorption and formation. Response of antiresorptive therapy is generally greatest with teleopeptides, intermediate with total pyridnolines and lowest with free pyridinolines.
CLINICAL UTILITY OF BONE MARKERS
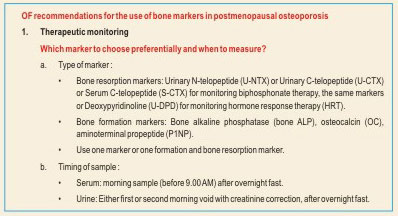
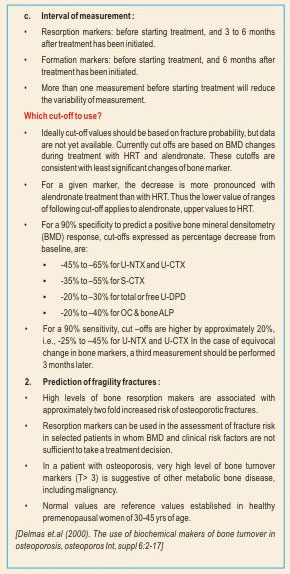
Therapy Monitoring
The most persuasive evidence to date for the use of bone markers is in the area of monitoring of osteoporosis treatment. The aim of the treatment is to prevent fractures. Biphosphonates, estrogens and ralozifene decrease bone resorption and bone formation markers.; strontium ravealte treatment causes a mild reduction in bone resorption markers and a slight increase in bone formation markers; teriparatide (recombinant PTH) increases both bone formation and bone resorption markers. The advantage of suing bone markers instead of BMD is the significant changes in the bone markers can be observed after three to six months after initiation of therapy, whereas changes in BMD becomes significant only after 18 to 24 months; a long time to detect treatment failure. The reduction in fracture risk following antiresorptive treatment was seen early similar to change in bone markers, whereas the change in BMD are gradual and later. No surprisingly change in bone markers explains a much greater proportion od reidction in fracture risk than any change in BMD. Taken together, these data suggest bone markers are arguably better tools than BDM for monitoring antiresorptive treatment.
Fractures risk assessment
The diagnosis of osteoporosis is based on bone density scanning by virtue of WHO definition of osteoporosis and patients with a low bone density have increased risk of fracture. However a considerable body of data indicates that bone markers predict bone markers predict bone loss independent of bone density; individuals with increased bone turnover loose bone at a faster rate than subjects with normal or low bone turnover markers. Bone turnover markers, in combination with other risks factors of osteoporosis fractures, may be used to describe fracture risk or intervention thresholds. The relative fracture risk, as defined by either low BMD or an increased bone turnover marker, I similar and increased fracture is accentuated when both are present. Thus, in clinical practice, increased bone turnover markers in the presence of a low BMD would favor initiation of treatment for that patient.
To identify noncompliant patient
Bone markers react very sensitively and quickly (within days) to irregular drug taking and therefore rapidly reveal inconsistent intake of medications. Positive feedback to the patient has been shown to improve the patient’s adherence to the prescribed medication. Studies have shown that up to 50% of patients stop treatment too early and medication is taken irregularly. Adherent patients were shown to suffer fewer fractures and to incur lower hospital costs.
To identify non responders to therapy
Most therapies are highly efficient as proven in many studies and true treatment failures are rare. However there are some patients who do not respond to therapy for the following reasons:
- Malabsorption
- Alcoholism
- Immobilization
- Glucocorticoid treatment
- Hyperthyroidism
Bone markers are able to identify these patents at a very early point in time to allow for appropriate measures to prevent future fractures.
FROM THE EDITOR’S DESK
 BIOCHMICAL MARKER of bone turnover are commonly used but underrated as tests in the management of bone disorders. Such tests do not establish the diagnosis of a disease, but rather they reflect the activity of the skeleton.
BIOCHMICAL MARKER of bone turnover are commonly used but underrated as tests in the management of bone disorders. Such tests do not establish the diagnosis of a disease, but rather they reflect the activity of the skeleton.
The utility of these markers in general practice is not well appreciated. In part this is because the results can vary if the tests are not appropriately done, casing frustration for some clinicians, who erroneously conclude that these markers lack utility.
In addition, there are opinions that the tests are not diagnostic, that they should not predict risk, and that they are not useful in patient management.
Wrong on all counts!
First of all these markers were never meant to diagnose a specific bone disease. They mayjorly reflect high bone activity or turnover or potential bone loss and high levels indicate that further assessment is needed. (in much the same way, an elevated prostate-specific antigen level may or may not mean the patient has prostate cancer, but it does not mean further assessment is needed.)
Second, these tests address fracture risk, either when used alone or when combines with bone densitometry measurements. A high level of a turnover marker indicates a risk of fracture similar to that of a T score lower than -2.5, with an odds ratio in the range of 2.4 to 2.8. Moreover, if a patient has a low T score and a high marker level, his or her risk is even higher, with an odds ratio of 4.1.
Third, the argument about the tests lack of ability to help in patient management is completely untrue, as these tests whether a bone physiology is responding to antiresorptive and anabolic drug therapy; marker activity should decline with antiresorptive drugs and increase the anabolic agents.
And this occurs months to years before bone densitometry even reflects a change!
The failure of test values to respond appropriately should prompt physicians to find out why. Is the patient not taking the medicine appropriately? Or more worrisome, is he or she not taking it at all?
Bone markers may be a solution to this dilemma. Changes in a bone marker help clinicians know that the patient is properly using therapy. Moreover, these changes tell the patient that treatment is working. In my experience, relaying this type of information to the patient encourages adherence. Studies have indicated that markers do indeed help patients stay adherent to therapy and avoid fractures. Hence, these markers can indicate the risk of fracture and are useful in managing patients and promoting compliance.
In this issue, Dr. Nimmi Kansal details the utility of these tests and emphasized the need to recognize that there is a valid reason for using these tests.
Also addressed in this issue are some frequently asked questions related to swine flu testing.
Your appreciative feedback is very encouraging and we look forward to suggestions to help us improve in our endeavor to provide you the best quality information in the field of diagnostics. We look forward to your participation and continued support.
Dr Reena Nakra
Chief Editor,
Chief of Lab and Zonal Lab Operations Heal
E-mail: reena.nakra@lalpathlabs.com