What it means to be Infertile in Men?
What is male infertility?
Male infertility is said to be the condition where in a male in incapable of impregnating a fertile female. Or in other words, the male unable to get a fertile female pregnant despite having meticulously timed unprotected sex for a period of one year.
A male is infertile if the number of sperms he ejaculates is less or the sperms which he ejaculates is of poor quality. Infertile males, will find difficulty in impregnating a fertile female and sometimes impossible in doing so.
Causes of male infertility
1) Sperm production problems: –
• Genetic problems
• Failure of testes to descend at birth
• Medicines and chemicals
• Infections
• Twisting of testes
• Radiation damage
• Unknown damage
2) Blockage of sperm transport: –
• Infections
• Prostate-related problems
• No presence of vas deferens
• Vasectomy
3) Sexual problems: –
• Premature ejaculation
• Ejaculation failure
• Erectile dysfunction
• Less frequency in sexual intercourse
• Injury to the spinal chord
• Prostate surgery
• Nerve damage
• Some medicines
4) Hormonal problems:-
• Tumours near the pituitary glands
• Pituitary problem at birth
• History of STDs
5) Sperm antibodies:-
• Vasectomy
• Injury
• Infection
• Unknown causes
6) Lifestyle: –
• Excessive consumption of alcohol
• Excessive consumption of tobacco
• Usage of drugs
• Exposure to radiation
• Exposure to poisonous or hazardous chemicals
• Wearing restrictive or tight underwear
Symptoms of male infertility
Considering the fact that just 7 out of 100 males are infertile, the symptoms of male infertility are often overlooked by men and they fail to notice the same. Here are a few common symptoms of male infertility that one needs to keep in mind.
• Difficulty in ejaculation
• Volume of ejaculated fluid is very less
• Significantly low sexual desire
• Erectile dysfunction
• Pain in testicle area
• Lumps in testicle area
• Swollen testes
• Frequent respiratory infections
• Loss of ability to smell
• Unusual breast growth
• Reduced facial hair
• Genital abnormality
• Hormonal abnormality
• Having a sperm count less than 15 million per ml of sperm or less than 39 million per ejaculation.
Diagnosis of male infertility (Male fertility test)
An initial male fertility test includes a thorough check up of medical history, a full body physical examination, extensive general hormone tests and one or more semen analysis tests, which measure the value of semen by volume as well as sperm count, ability of sperms to move spontaneously and quality of sperm motion.
Medical history test
A medical history test is mandatory in course of a male infertility test. This includes
• A thorough review of previous medical conditions, past medical history, surgeries prior to the infertility test, previously administered medication
• An in depth consider family history regarding infertility and birth defects
• A meticulous review of social history, workplace hazards to evaluate the hazards a male is exposed to that could affect fertility and lead to infertility.
Full body physical test
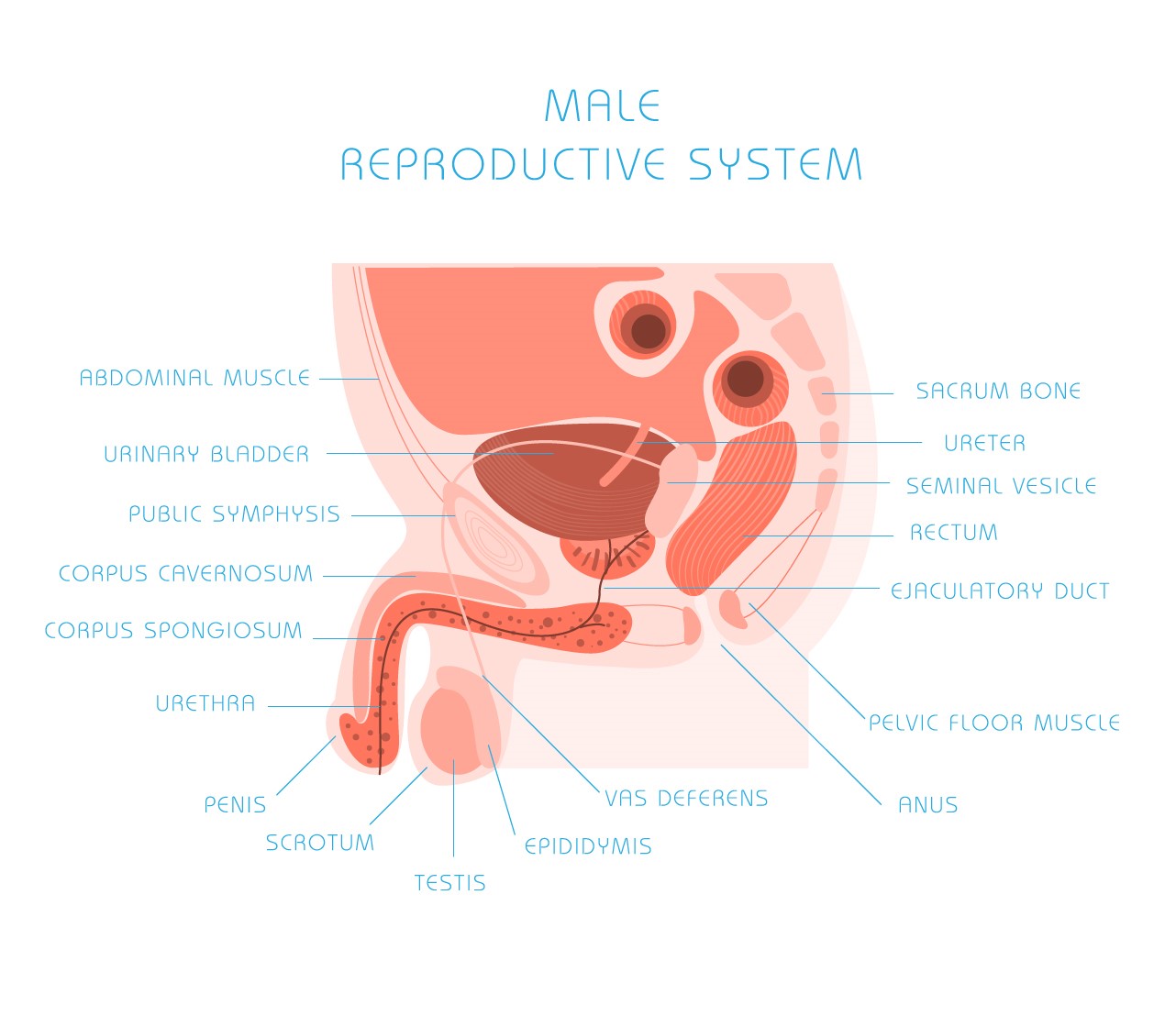
This is also an integral part of male infertility test. It consists of an elaborate full body test which includes special attention to pelvic organs such as penis, testes, scrotum and prostate.
Laboratory tests
This is the most crucial part of male infertility test. These include
• Urinalysis – To detect the presence of any infections
• Semen Evaluation – This is done to evaluate sperm mobility, sperm shape, sperm shape, volume of the ejaculate, sperm count and the liquidity and viscosity of the ejaculate
• Hormonal tests – This test evaluates the levels of testosterone and FSH (follicle-stimulating hormone) which maintains the general equilibrium of the hormonal system and sperm production. Serum LH and prolactin are other hormonal tests that may be done if clear inferences cannot be drawn from the initial tests.
If these tests do not provide substantial evidence of infertility, the following tests will be performed
• Seminal Fructose Test — To find out if fructose is being added adequately to the semen by the seminal vesicles
• Post-ejaculate Urinalysis — To determine if there is any obstruction during ejaculation
• Semen Leukocyte Analysis — To ascertain the presence of white blood cells in the semen
• Kruger and World Health Organization (WHO) Morphology — This test is performed to examine the shape of the sperm and its features in detail
• Anti-sperm Antibodies Test — To ascertain the presence of antibodies that may lead to infertility
• Sperm Penetration Assay (SPA) — To ascertain the ability of the sperm to fertilize
• Ultrasound — To detect gnarled or enlarged veins or duct obstructions in the prostate, scrotum, seminal vesicles and ejaculatory ducts
• Testicular Biopsy — To detect if sperm production is impaired or if a blockage exists
• Vasography — To determine the structure of the duct system and find out the presence of any obstructions
• Genetic Testing — To rule out fundamental mutations in one or more gene regions of the Y genetic material, or to test for cystic fibrosis in men absent the vas deferens
Treatment for infertility in men
Any treatment to increase fertility may be expected to have a direct outcome on semen quality approximately three months after its beginning, as this is the time essential for a single cycle of spermatogenesis, or sperm production. If neither surgical nor medical therapy is suitable, assisted reproductive technologies are possible.
In choosing a treatment plan, thought should be given to each couple’s long-standing goals, financial constraints, and the results of the female partner’s assessment in addition to male factor results.
Specific Therapy
This is by far the most successful medical therapy for curing male infertility. It involves reversing chemicals, infections or endocrine imbalances. This is known as specific therapy, and is usually successful because this treatment is based on the rectification of well-defined problems.
Examples of specific therapy may include:
• Treatment for mild prostatitis, epididymitis or varicocele
• The substitute of the pituitary hormones — follicle stimulating hormone (FSH) and leutinizing hormone (LH) — for radiation or surgically induced pituitary ailment
• The administration of male sex hormone (testestorone) in men with hypoandrogenic hypogonadism
Empiric Therapy
Empiric thrapy is another kind of treatment, that is aimed at correcting quite ill-defined conditions. The making use of of clomiphene citrate, tamoxifen or ProXeed for low sperm concentration or motility are instances of this form of therapy.
These treatments generally have limited success because the generally intact mechanisms within the body tend to resist the planned effect. In other words, hormonal treatments based on the theory that “if some hormone is good, then more is better” are predestined to letdown and must be avoided at any expense.
Assisted Reproductive Technology
Obtaining treatment for certain illnesses may or may not be a solution to the fertility problem. It has been gauged that at least 10 percent of infertility problems have been found out to occur due to unfamiliar causes and another 30 percent are due to trouble in both the male and female partners.
In addition to medicine and surgical infertility treatments to take care of specific health conditions in men, a latest class of treatments — called Assisted Reproductive Technologies, or ART — has been introduced. The most familiar ART is In Vitro Fertilization, or IVF, but new procedures can boost the IVF process or address other infertility circumstances. These procedures for men include:
• Intracytoplasmic sperm injection (ICSI)
• Sperm withdrawal procedures, such as:
Vasal aspiration
Epididymal aspiration
Testicular sperm extraction
“Mapping” the flawed testes
• Sperm donors and embryo or semen freezing
Intracytoplasmic Sperm Injection (ICSI)
Intracytoplasmic sperm injection, or ICSI, is a method that has been developed to help achieve fertilization for couples with infertility from the male’s end or even couples who had earlier failed to fertilize in a prior in vitro fertilization effort. This particular procedure overcomes many of the barriers to fertilization and allows couples with little or no hope of achieving successful pregnancy to obtain fertilized embryos.
Sperm Extraction Procedures
Sperm Extraction (Vasal Aspiration ) : Patients who have congenital impediment of the ductal system at the level of the prostate or in the abdominal or pelvic portions of the vas deferens may make the most of this method. Patients who have undergone a vasectomy within less than five years may also make use of this method to become fertile again.
• Sperm Extraction ( Epididymal Aspiration ): Epididymal sperm aspiration may be performed in instances in the absence of vas deferens or a vas defrens scarred due to prior surgery, trauma or infection. Sperms are directly accumulated from a single, lonely epididymal tubule (MESA) or by blind needle puncture (PESA) in almost the same method as the vasal procedure. Subject to the length of the epididymis that is obtainable for aspiration, multiple, different aspiration attempts can be made from one or both the testes.
• Sperm Extraction: Testicular Sperm Extraction (TESE); Testicular Sperm Aspiration (TESA): The latest of the aspiration techniques in testicular sperm retrieval. In this process, a small quantity of testis tissue is obtained by biopsy under the influence of local anaesthesia. It is a burst through in that it demonstrates that sperm do not have to “mature” and travel through the epididymis to fertilize an ovum egg. Because of their lack of maturity, however, testicular sperm need ICSI.
Visit your nearest Dr Lal PathLabs or book a test online from the Dr Lal PathLabs mobile app for collection of samples from any place of your choice and convenience of tests related to male infertility.